Not only do the wearable sensors track movement to detect falls illustrated above, but similar technology is integrated into an interactive balance training program that offers additional value in post-stroke or cardiac arrest rehabilitation [Journal of NeuroEngineering and Rehabilitation].
University of Arizona researchers were awarded a $1.5 million Phase II Small Business Innovation Research (SBIR) grant from the National Institutes of Health to develop an Upper Extremity Frailty Device to identify elderly patients who may be at high risk for certain medical treatments.
The Interdisciplinary Consortium on Advanced Motion Performance (iCAMP) and the Division of Trauma Surgery in the UA Department of Surgery, and the Arizona Center on Aging (ACOA) are collaborating on a mobile system to assess frailty based on a brief arm movement task. This technology would replace existing tools that are too time-consuming for routine clinical use or are impractical for mobility-impaired patients.
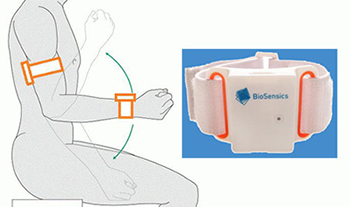 A wearable sensor includes a tri-axial gyroscope and a tri-axial accelerometer. The elbow is moved up and down for 20 seconds to obtain a reading. The raw data are processed and a frailty score assigned based on findings.
A wearable sensor includes a tri-axial gyroscope and a tri-axial accelerometer. The elbow is moved up and down for 20 seconds to obtain a reading. The raw data are processed and a frailty score assigned based on findings.
To date, frailty screening has required lengthy questionnaires, or gait assessment, both of which are difficult to perform in busy clinical settings or on patients who are bed-bound. The Upper Extremity Frailty Device takes less than 1 minute and is highly sensitive and specific to the gold standard “Fried Frailty” criteria, which consists of measuring fatigue, weight loss, gait speed, exhaustion and inactivity.
Frailty is a state of excess vulnerability. Frailty screening helps to identify older adults at high risk of a lengthy hospital stay, poor surgical outcomes, re-hospitalization or institutionalization and who are at high risk of mortality. By knowing the frailty level of the patient (frail, pre-frail or non-frail), medical practitioners can better predict likely outcomes, prescribe appropriate treatment and customize discharge that aligns with the patient’s goals and values, said Nima Toosizadeh, PhD, an iCAMP post-doctoral fellow and a member of the research team, who helped lead the validation study of the technology.
Bijan Najafi, PhD, professor and iCAMP director, and Bellal Joseph, MD, associate professor in the Division of Trauma, Critical Care, Burn and Emergency Surgery, are principal investigators of the study and are collaborating with Banner Sun Health researchers to test this device across various settings, including in the home, outpatient clinics and in the hospital as part of pre- and post-surgical care.
The grant, submitted with the company BioSensics, LLC (Cambridge, Mass.), will be used to refine the Upper Extremity Frailty Device graphical user interface for future commercialization. A patent also has been filed and successfully licensed by industry.
“Rapid advances in development of ‘precision,’ wearable technologies and mobile health are allowing health-care providers to objectively track health status, as well as response to an intervention. For the first time, we have designed and validated an innovative and practical wearable technology that could assist providers to objectively track frailty status of their patients and provide personalized care,” said Dr. Najafi,
“Emerging mobile and wearable technologies provide an effective, flexible and integrative solution for monitoring and measuring the different aspects of frailty in real-life settings,” he said.
Practical, low-cost devices that can help providers and health-care systems identify risks of older adults are needed. This Upper Extremity Frailty Device is highly relevant, and has great potential to help optimize care strategies, while minimizing costs, said Jane Mohler, RN, MPH, PhD, professor of medicine and associate director of ACOA and iCAMP, a key investigator on this study.
Dr. Joseph said, “The population is changing as well as the way we deliver care. This is yet another example of the importance of collaborating across multiple disciplines. Dr. Najafi and Mohler and their teams are revolutionizing the way health care is being practiced. When it’s all said and done, the patients will be the ultimate winners.”


