 Two renowned genetic and genomic medical investigators have been recruited to the University of Arizona College of Medicine – Tucson to head new divisions within the UA Health Sciences that focus on research aimed at helping develop precision medicine solutions to diseases from asthma to cancer to diabetes and beyond.
Two renowned genetic and genomic medical investigators have been recruited to the University of Arizona College of Medicine – Tucson to head new divisions within the UA Health Sciences that focus on research aimed at helping develop precision medicine solutions to diseases from asthma to cancer to diabetes and beyond.
 Eugene R. Bleecker, MD, and Deborah A. Meyers, PhD, will serve as professors of medicine, co-chiefs of the new Division of Genetics, Genomics and Precision Medicine within the Department of Medicine and co-directors of the new Division of Pharmacogenomics in the UA Center for Applied Genetics and Genomic Medicine.
Eugene R. Bleecker, MD, and Deborah A. Meyers, PhD, will serve as professors of medicine, co-chiefs of the new Division of Genetics, Genomics and Precision Medicine within the Department of Medicine and co-directors of the new Division of Pharmacogenomics in the UA Center for Applied Genetics and Genomic Medicine.
 “I’m very excited that Drs. Bleecker and Meyers have joined the UA,” said Department of Medicine Chair Monica Kraft, MD, who is also The Robert and Irene Flinn Endowed Professor of Medicine and deputy director, UAHS Asthma and Airway Disease Research Center (A2DRC). “They have been colleagues and collaborators for years and their work has been groundbreaking in helping our field better understand the genetics behind asthma and chronic obstructive pulmonary disease (COPD). They have inspired my own research and countless other investigators seeking more personalized remedies to provide relief for our patients from respiratory illnesses, diabetes, prostate cancer and several other diseases.”
“I’m very excited that Drs. Bleecker and Meyers have joined the UA,” said Department of Medicine Chair Monica Kraft, MD, who is also The Robert and Irene Flinn Endowed Professor of Medicine and deputy director, UAHS Asthma and Airway Disease Research Center (A2DRC). “They have been colleagues and collaborators for years and their work has been groundbreaking in helping our field better understand the genetics behind asthma and chronic obstructive pulmonary disease (COPD). They have inspired my own research and countless other investigators seeking more personalized remedies to provide relief for our patients from respiratory illnesses, diabetes, prostate cancer and several other diseases.”
Their roles at the UA will allow them to apply their approaches to many diseases that will move precision medicine to the next level, she added. Kenneth S. Ramos, MD, PhD, PharmB,  interim dean, UA College of Medicine – Phoenix, and UAHS associate vice president, Precision Health Sciences, and director, UAHS Center for Applied Genetics and Genomic Medicine, agreed.
interim dean, UA College of Medicine – Phoenix, and UAHS associate vice president, Precision Health Sciences, and director, UAHS Center for Applied Genetics and Genomic Medicine, agreed.
“Their leadership and contributions in the areas of pharmacogenomics and personalized medicine will be invaluable as the Center continues to advance precision medicine at the UA Health Sciences and Banner – University Medicine Division,” he said. “We look forward to working closely with both of them to integrate their expertise with those of other divisions within the Center and to implement innovative programs in the area of pharmacogenomics.”
Pushing the Edge of Genetics Evolution
In Winston-Salem, N.C., Drs. Bleecker and Meyers were professors and co-directors of Wake Forest University’s Center for Genomics and Personalized Medicine. He also was Wake’s Thomas H. Davis Professor of Medicine in the Internal Medicine Section on Pulmonary, Critical Care, Allergy and Immunologic Diseases—of which he was section chief from 2002-09.
They are both part of several national research networks—often since their inception—with a focus on genetic and genomic research, frequently related to respiratory diseases. These include AsthmaNet, COPDGene®, the Eve Consortium, the Severe Asthma Research Program (SARP), SPIROMICS, and the Trans-Omics for Precision Medicine (TOPMed) Program. They’re also part of a UAHS application for the Precision Interventions for Severe and/or Exacerbation Prone Asthma (PrecISE) Program, for which funding has not yet been awarded.
In their careers, they’ve been awarded grants valued at nearly $125 million, most from the National Institutes of Health’s National Heart, Lung and Blood Institute. From that research, she authored more than 350 scientific manuscripts, he more than 400—often collaboratively. In all, Wake Forest investigators at their center published nearly 1,200 papers since its 2000 inception as part of a $67 million research initiative. Topics split evenly among respiratory, diabetes and cancer.
“We interact with a number of other groups, but our major focus has been on the genetics of asthma and susceptibility of asthma and COPD,” Dr. Bleecker said. “Our particular interest is whether other genetic influences interact with the environment and cause disease progression. As part of that, we’ve become pretty good phenotypers in both asthma and COPD… And Deb is among the top geneticists who really emphasize asthma and COPD.”
From Biomarkers to Whole-Genome Sequencing
Dr. Meyers notes the ability of whole-genome sequencing—calculating the complete DNA sequence of an organism at one time—to determine susceptibility of a specific person to a particular disease often requires a broader look at familial genetic traits and medical history. That’s why their most recent grant applications, such as TOPMed, focus on acquiring sets of data for thousands of individuals to find patterns that identify or confirm genetic markers contributing to certain medical conditions. From these biomarkers, clinical researchers increasingly are able to further development of therapies tailored for groups of people or even individuals.
With more limited information, though, Dr. Meyers acknowledged sometimes even a negative family history can be “non-informative,” using as an example breast cancer, which has clear biomarkers (BRCA1 and BRCA2) that can be revealed by genetic testing.
“Depending on whether you’re looking at large families, the genes don’t always show themselves. That’s the rationale on why you’d like to do more extensive genetic testing of more individuals, to be certain you’ve got an informed family history,” she said.
“With me for instance, I don’t have any sisters. My mother’s still alive, but she doesn’t have sisters. My dad was an only child. You don’t know in that case. You’ve got to give those genes a chance to show themselves.”
The same may be true for prostate cancer.
“There’s some compelling data,” Dr. Bleecker said. “There are families in which half of the men have prostate cancer. Again, your risk is not just because your father and your uncle had prostate cancer, but whether you inherited the genetic variants that give you susceptibility. That’s where predictive testing is helpful.”
Family vs. Lifestyle, Environment
But possessing biomarkers alone in one’s genetic makeup doesn’t mean a person will get a disease. Sometimes environment or lifestyle is just as important. The TOPMed grant they’ve applied for would give them genetic datasets on 4,000 subjects with smoking-related disease, including whole-genome sequencing and RNA sequencing longitudinally (i.e., over years or decades). One thing they plan to look at is why some smokers develop COPD and emphysema—while others don’t.
The cost of genetic testing, which can be as much as a few thousand dollars, depending on the nature and complexity of tests, make it expensive for most individuals. Still, Dr. Meyers said many people are paying for such testing because it’s “not just about yourself, but about your family and finding out your family members’ genetic risks.”
 Drs. Bleecker and Meyers have seen a lot of advances in better understanding the genetics behind respiratory diseases and been part of all the major U.S. studies and several international ones.
Drs. Bleecker and Meyers have seen a lot of advances in better understanding the genetics behind respiratory diseases and been part of all the major U.S. studies and several international ones.
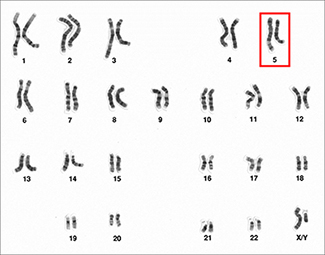
“We first used family studies with a New England Journal of Medicine paper to say there was a region on chromosome 5 (see image at left) with genes that control inflammation related to asthma susceptibility. At the time, we had more limited genetic markers. Then, we moved into what we call GWAS, or genome-wide association studies. We published early papers on genetic susceptibility for asthma using GWAS and, now, we’re involved in the NHLBI program, TOPMed. For GWAS, we use chips with hundreds of thousands of markers, and have now moved to whole-genome sequencing.”
Tracking Respiratory Illnesses' Roots
Dr. Meyers was first author on a 2014 paper that appeared in Lancet Respiratory, “The Genetics of Asthma: Towards a Personalized Approach to Diagnosis and Treatment,” which highlights the advances made toward personalizing therapies for asthma based on genotype profiling— determining the genetic makeup of an individual by examining their DNA sequence. A survey of more recent papers shows them addressing topics such as “Effects of age and disease severity on systemic corticosteroid responses in asthma” and “Meta-analysis of asthma-related hospitalization in mepolizumab studies of severe eosinophilic asthma.”
Dr Bleecker is very active in clinical trials on the efficacy of therapies to address asthma and COPD, including two studies published last summer in The Lancet that looked at how “Benralizumab injections reduce exacerbations in severe, uncontrolled asthma” and in NEJM on “Serious asthma events with budesonide plus formoterol vs. budesonide alone.” They plan to continue to participation of patients in their research at the UA.
Precision Medicine & 'Good Science in Arizona'
In fact, both are excited to collaborate with others here because of the “very good science going on at Arizona.” They’ve associated closely with a number of UA Health Sciences faculty at the American Thoracic Society, through their research and as guest speakers invited to present on their work in Tucson.  This includes at the Winter Lung Series Conference, hosted by the A2DRC and UA Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, and the Problems in the Biology of Complex Diseases Colloquium, coordinated by Donata Vercelli, MD, director of the Arizona Center for the Biology of Complex Diseases at the UA BIO5 Institute.
This includes at the Winter Lung Series Conference, hosted by the A2DRC and UA Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, and the Problems in the Biology of Complex Diseases Colloquium, coordinated by Donata Vercelli, MD, director of the Arizona Center for the Biology of Complex Diseases at the UA BIO5 Institute.
The two are enthusiastic about exploring expansion of their research with several existing and new UAHS research centers, including the UA Cancer Center; Center for Disparities in Diabetes, Obesity and Metabolism; Center for Innovation in Brain Science; Center for Border Health Disparities; Center for Population Science and Discovery; Arizona Institute for Clinical and Translational Science; Center for Biomedical Informatics and Biostatistics, as well as the All of Us℠/Precision Medicine Initiative (PMI).
 Arizona All of Us℠/PMI lead principal investigator Akinlolu O. Ojo, MD, MPH, PhD, said he welcomes their input. “There will be vast opportunities for rapid innovations and discoveries that directly benefit our patients in this landmark effort—which is the largest NIH peer-reviewed grant in state history—to enroll 1 million or more participants nationwide who will contribute their health information and biological specimens to create a rich resource for researchers to leverage to identify better ways to prevent and treat diseases, tailored to individual health needs, genetics, environment and lifestyle.”
Arizona All of Us℠/PMI lead principal investigator Akinlolu O. Ojo, MD, MPH, PhD, said he welcomes their input. “There will be vast opportunities for rapid innovations and discoveries that directly benefit our patients in this landmark effort—which is the largest NIH peer-reviewed grant in state history—to enroll 1 million or more participants nationwide who will contribute their health information and biological specimens to create a rich resource for researchers to leverage to identify better ways to prevent and treat diseases, tailored to individual health needs, genetics, environment and lifestyle.”
Population Studies & Ongoing Collaborations
Drs. Bleecker and Meyers note they’ll also continue to work with research partners at Wake Forest, Emory University and other institutions, where grants call for larger or specific population studies. Their ongoing research, for example, includes studies into “genetics of lung function and asthma severity in African Americans,” “longitudinal phenomics and genetics of severe asthma,” “immunopathogenesis associated with fungal asthma severity,” and “systems pharmacogenomics of asthma treatment.”
They have collaborated together since meeting in 1978 in Baltimore at Johns Hopkins University, where he was director of the Division of Pulmonary and Critical Care at Baltimore City Hospital and they both were assistant professors. In 1989, he became pulmonary section chief at the Baltimore Veterans Administration Medical Center and, in 1996, director of the Center for the Genetics of Asthma and Complex Diseases at the University of Maryland, also in Baltimore.
She was a geneticist at Johns Hopkins and a Howard Hughes Medical Institute investigator, and left Johns Hopkins to join Dr. Bleecker at the University of Maryland as the center’s associate director in 1997 and director of the Program in Human Genetics. In 2000, they both joined the faculty at Wake Forest to launch what was then the Center for Human Genomics.
Background & Honors
Drs. Bleecker and Meyers both earned their undergraduate degrees in biology, he from New York University and she from Ithaca College. He earned his medical degree from State University of New York – Brooklyn College of Medicine, afterward completing an internship and residency in internal medicine at Brooklyn’s Kings County Hospital Center, a second residency at Baltimore’s Johns Hopkins Hospital and a pulmonary disease fellowship at the University of California – San Francisco. She earned her doctorate in medical genetics at the Indiana University School of Medicine and completed a postdoctoral fellowship in biostatistics and genetics at the University of North Carolina – Chapel Hill.
Dr. Meyers also was an associate editor of the journal Human Genetics, European Respiratory Journal and Journal of Allergy and Clinical Immunology, as well as a past member of the NIH International and Cooperative Projects Study Section and NIH Center for Inherited Disease Research Study Section. In 2005, she was presented with the senior science award from the Sandler Foundation, established by ProPublica founders Herbert and Marion Sandler.
Dr. Bleecker serves on the editorial board of the Journal of Allergy and as chair of the Asthma Committee of the World Allergy Organization and an elected Scientific Council Member of the Collegium Internationale Allergologicum, founded in Milwaukee in 1954 by a group of distinguished physicians and scientists in medicine and the emerging field of allergy and clinical immunology.
Joining them at the UA from Wake Forest is Xingnan Li, PhD, now an assistant professor of medicine in the UA Division of Genetics, Genomics and Precision Medicine. Dr. Li completed his undergraduate degree at Peking University, before earning a doctorate and master’s degree at Michigan State University. Having both a doctorate in genetics and a master’s degree in biostatistics makes him a critical member of the new division. He has more than 100 published papers to his credit on related research.
Drs. Bleecker and Meyers said they are actively recruiting other physicians and investigators.
About the UA College of Medicine – Tucson
The University of Arizona College of Medicine – Tucson is advancing health and wellness through state-of-the-art medical education programs, groundbreaking research, and advancements in patient care in Arizona and across the United States. Founded in 1967, the College ranks among the top medical schools in the nation for research and primary care and is leading the way in academic medicine through its partnership with Banner – University Medicine, a new division of one of the largest nonprofit health-care systems in the country. For more information: http://medicine.arizona.edu
About the University of Arizona Health Sciences
The University of Arizona Health Sciences is the statewide leader in biomedical research and health professions training. The UA Health Sciences includes the UA Colleges of Medicine (Phoenix and Tucson), Nursing, Pharmacy and Mel and Enid Zuckerman College of Public Health, with main campus locations in Tucson and the growing Phoenix Biomedical Campus in downtown Phoenix. From these vantage points, the UA Health Sciences reaches across the state of Arizona and the greater Southwest to provide cutting-edge health education, research, patient care and community outreach services. A major economic engine, the UA Health Sciences employs almost 5,000 people, has nearly 1,000 faculty members and garners more than $126 million in research grants and contracts annually. For more information: http://uahs.arizona.edu. Follow us: Facebook | Twitter | YouTube | LinkedIn

