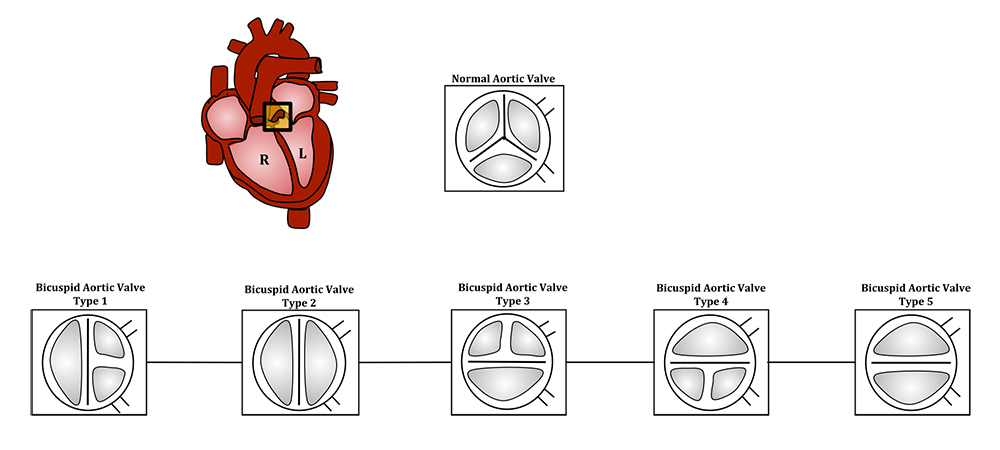
Normal versus bicuspid aortic valve: The aortic valve controls outflow of blood from the left ventricle of the heart through the aorta (valve is indicated within the yellow highlighted box). Normal aortic valve is tricuspid. Five types of bicuspid valve are shown, with Type 1 being most prevalent. Bicuspid valve forms when the tissue surrounding one of the cusps (leaflets) of the valve fuse during fetal development. This developmental anomaly can have either negative or no effect on the individual. (Source: Lcaron101/Wikimedia)
 The University of Arizona Structural Heart Disease Program team at Banner – University Medical Center Tucson reached another milestone last week in completing the first-ever transcatheter aortic valve replacement (TAVR) procedure on a patient with a bicuspid aortic valve utilizing only transesophageal echocardiography (TEE) to guide them.
The University of Arizona Structural Heart Disease Program team at Banner – University Medical Center Tucson reached another milestone last week in completing the first-ever transcatheter aortic valve replacement (TAVR) procedure on a patient with a bicuspid aortic valve utilizing only transesophageal echocardiography (TEE) to guide them.
The procedure also was unique in that only a minimum of contrast dye was employed in final diagnoses preparations for the procedure and no CT (computed tomography) scan was used at all.
Structural heart team for this procedure (on right): From left, Dr. Ranjith Shetty (interventional cardiologist); Dr. Toshinobu Kazui (cardiac surgeon); Dr. George Gellert (cardiac anesthesiologist); Dr. Paul Ford (cardiac anesthesiologist); Dr. Sam Paidy (cardiac anesthesiologist) and Dr. Kapildeo Lotun (interventional cardiologist), director, Structural Heart Disease Program.
Two TAVR procedures were completed on Wednesday, Oct. 3, on elderly male patients, one from Arizona and one from out of state. Each procedure took about 1.5-2 hours. The bicuspid aortic valve patient was from New Mexico and also suffered from kidney disease. He was released the next day from the hospital and is now back home.
“He was not on hemodialysis. We were trying to prevent him from having to go on dialysis. That’s one of the reasons we minimized use of the contrast dye,” noted Monique Crawford, RN, a clinical coordinator for the program. “We didn’t want to tip him over the edge with that potential reaction.”
 Bicuspid aortic valves are a congenital heart defect involving an inherited form of heart disease where two of the leaflets of the aortic valve fuse during development in the womb resulting in a two-leaflet (or bicuspid) valve instead of the normal three-leaflet (or tricuspid) valve—see illustration at top of this article. This is the most common cause of heart disease present at birth and affects about 1.3 percent of adults, according to the New England Journal of Medicine. In many cases, a bicuspid aortic valve will cause no problems. Those with this condition, however, may become tired more easily and find it difficult to maintain stamina for strenuous activities due to poor heart performance.
Bicuspid aortic valves are a congenital heart defect involving an inherited form of heart disease where two of the leaflets of the aortic valve fuse during development in the womb resulting in a two-leaflet (or bicuspid) valve instead of the normal three-leaflet (or tricuspid) valve—see illustration at top of this article. This is the most common cause of heart disease present at birth and affects about 1.3 percent of adults, according to the New England Journal of Medicine. In many cases, a bicuspid aortic valve will cause no problems. Those with this condition, however, may become tired more easily and find it difficult to maintain stamina for strenuous activities due to poor heart performance.
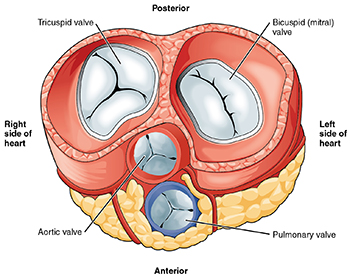
Heart valves illustration from Anatomy & Physiology. See the aortic valve on the lower left side. (Source: Connexions/Wikimedia)
When treatment is necessary, normally, contrast dye is administered during preparatory steps for diagnoses as well as during the procedure to help identify where physicians are placing the valve via this minimally invasive procedure. About 100 ml of dye is used in each of three steps: first, during cardiac catheterization for an angiogram; second, during a CT scan and, finally, during the procedure itself. Again, here, only about 25 ml of dye was used in the first step and the second step was skipped altogether.
“Yesterday, our team with the assistance of George Gellert, MD (Banner – University Medical Center Phoenix) implanted a tanscatheter aortic replacement valve utilizing only TEE guidance in a patient with bicuspid aortic valve who suffers from kidney disease,” said  Kapildeo Lotun, MD (right), a professor of medicine in the UA Division of Cardiology, director of the Structural Heart Disease Program and Vascular Medicine at the UA Sarver Heart Center, and director of the Catheterization Laboratory at Banner – UMC Tucson.
Kapildeo Lotun, MD (right), a professor of medicine in the UA Division of Cardiology, director of the Structural Heart Disease Program and Vascular Medicine at the UA Sarver Heart Center, and director of the Catheterization Laboratory at Banner – UMC Tucson.
“In utilizing this alternative imaging modality, our team was able to complete the pre-procedure diagnostic testing and implant the TAVR valve using less than 30 ml of contrast dye, allowing for increased renal protection and preservation of the patient’s renal function,” Dr. Lotun added.
Dr. Gellert is a cardiac anesthesiologist and medical director of Interventional Echocardiography at Banner – UMC Phoenix and a clinical assistant professor of anesthesiology at the UA College of Medicine – Phoenix. He also serves on faculty at Creighton University School of Medicine and Mayo Clinic College of Medicine. Dr. Gellert’s imaging courses and on-site proctoring have provided both surgical and interventional 3D-echocardiography education and hands-on training to hundreds of cardiologists, cardiac anesthesiologists and cardiac sonographers across the United States. He is a consultant, trainer and proctor for Edwards LifeSciences THV, HVT, ET and CC; Medtronic HVT TAVR Global Field Team; Abbott Structural MitraClip; Philips HealthCare US; Siemens Medical US and GE Healthcare US, and serves as chief imaging advisor for Mardil Medical. He has been in private practice for 24 years with Valley Anesthesiology Consultants in Phoenix.
Dr. Gellert was impressed with the UA/Banner team on these two TAVR procedures.
“They just wanted to absolutely rely on what I do with TEE, or echo, to guide them on implantation,” he said. “The other uniqueness was there was no CT done at all, no contrast on the TAVR and no bicuspid valve patient done without contrast previously. I’m pretty much one of the only proctors that go around the country to do these and I’ve never proctored a case like this where no CT was done… so it’s truly a unique undertaking.” Twice.
Dr. Lotun noted the second procedure, while not as challenging due to the first patient’s extenuating circumstances and the type of aortic valve involved, was also completed with minimal or no contrast dye use and no CT scan, using only echocardiography to assist them in placing the replacement valve.
“Our team would like to thank Dr. Gellert for his time and expertise,” Dr. Lotun said. “We are excited to continue to utilize the skills he has shared with us. These skills will allow us to provide individualized care for patients with decreased renal function and valvular disease.”
Others involved in the procedures included Ranjith Shetty, PhD, assistant professor, Division of Cardiology, associate director, Structural Heart Disease Program, and associate director, TAVR Program; Toshinobu Kazui, MD, PhD, assistant professor, UA Department of Surgery; Paul Ford, MD, assistant professor, UA Department of Anesthesiology; Sam Paidy, MD, assistant professor, UA Department of Anesthesiology and director of cardiac anesthesia,  and Kristie Fry, ACNP-BC (left), nurse practitioner in the Structural Heart Disease Program.
and Kristie Fry, ACNP-BC (left), nurse practitioner in the Structural Heart Disease Program. 
Dr. Lotun also thanked the cath lab staff and structural heart coordinators Crawford and Devan V. Lodge, RN, CCRN, for their contributions. In April, the team completed the program’s 300th TAVR procedure at Banner – UMC Tucson. The first-ever TAVR procedure at the hospital was performed in August 2012.
For more information regarding our structural heart therapies call (520) 626-8578. For general clinical questions or appointments involving heart care, please call (520) MyHeart (694-3278) or (520) 626-2000. You also can visit the UA Sarver Heart Center’s Heart Health webpage to learn more.
ALSO SEE:
“UA Structural Heart Team Completes 300th TAVR Procedure in Little More than Five Years” | Posted April 9, 2018

