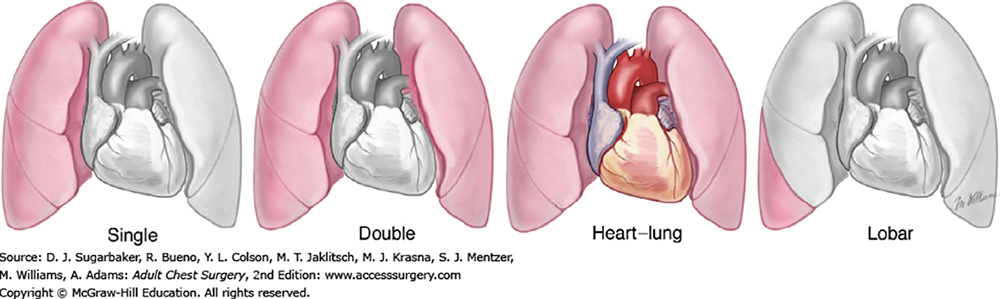
Types of lung transplantation (Source: AccessSurgery - McGraw-Hill Medical)
 Physicians at the University of Arizona College of Medicine – Tucson can take a large amount of credit for recent news that Banner – University Medical Center Tucson has been recognized by the Blue Cross Blue Shield Association as a Blue Distinction Center® of excellence for lung transplants.
Physicians at the University of Arizona College of Medicine – Tucson can take a large amount of credit for recent news that Banner – University Medical Center Tucson has been recognized by the Blue Cross Blue Shield Association as a Blue Distinction Center® of excellence for lung transplants.
 The Blue Cross Blue Shield Association is a federation of 36 U.S. health insurance organizations and companies providing coverage to more than 106 million people.
The Blue Cross Blue Shield Association is a federation of 36 U.S. health insurance organizations and companies providing coverage to more than 106 million people.
This recognition comes on the heels this past winter of recognition for the hospital and lung transplant program as an Aetna Institutes of Excellence™ Transplant Facility. About 38.8 million people rely on Aetna to help them make decisions about their health care and health care spending.
So far this year, there have been 35 lung transplant procedures completed at Banner – UMC Tucson, a 50 percent jump in the number done in all of 2017.
A Team Effort
The Lung Transplantation Program at the hospital is overseen by a multidisciplinary team of physicians and staff that includes pulmonologists, surgeons, transplant specialists, respiratory therapists, nurses, social workers and more at both Banner – UMC Tucson and Banner – UMC Phoenix, which refers lung transplant candidates to Tucson.
 Steven R. Knoper, MD, a UA assistant professor, transplant pulmonologist and co-medical director of the Banner – UMC Tucson Lung Transplantation Team, said, “This achievement is a credit to the teamwork of our Phoenix and Tucson campus clinical teams, in collaboration with our administrative partners, which allowed us to meet volume and quality measures necessary for this distinction.”
Steven R. Knoper, MD, a UA assistant professor, transplant pulmonologist and co-medical director of the Banner – UMC Tucson Lung Transplantation Team, said, “This achievement is a credit to the teamwork of our Phoenix and Tucson campus clinical teams, in collaboration with our administrative partners, which allowed us to meet volume and quality measures necessary for this distinction.”
He added, “It is another insurance contracting milestone that will let us provide lung transplant for our patients with this insurance product. Congratulations for the hard work by all involved in this achievement.”
Credit to Spare
Dr. Knoper made a point of thanking others involved in the effort for their hard work in successfully turning up the volume on the lung transplant program since it was credentialed again by the Centers for Medicare & Medicaid Services (CMS) in the fall of 2016.
 Among those, he said, have been Monica Kraft, MD (on left at right), professor and chair, UA Department of Medicine; Sairam Parthasarathy, MD (middle at right), professor and interim chief, UA Division of Pulmonary, Allergy, Critical Care and Sleep Medicine (PACCS); Joshua Malo, MD, a transplant pulmonologist and assistant professor, PACCS; Darryl Lundeen, MSHA, BSN, RN, transplant services director, Banner – UMC Tucson, and Sarah Frost (far right, above right), CEO of Banner – University Medical Centers Tucson and South.
Among those, he said, have been Monica Kraft, MD (on left at right), professor and chair, UA Department of Medicine; Sairam Parthasarathy, MD (middle at right), professor and interim chief, UA Division of Pulmonary, Allergy, Critical Care and Sleep Medicine (PACCS); Joshua Malo, MD, a transplant pulmonologist and assistant professor, PACCS; Darryl Lundeen, MSHA, BSN, RN, transplant services director, Banner – UMC Tucson, and Sarah Frost (far right, above right), CEO of Banner – University Medical Centers Tucson and South.
“Many of us remember the sad day in 2012 when the hospital inactivated its struggling lung transplant program,” Frost said. “Now, our program is not just back on track, but winning national distinctions. The steady growth and clinical success of our lung transplant program over the past few years is one of our proudest accomplishments. Congratulations and thank you to the entire transplant team.”
 Others Dr. Knoper recognized include Scott Lick, MD, UA professor of surgery and surgical director of the Heart and Lung Transplant program at Banner – UMC Tucson; Rajeev Saggar, MD, UA clinical associate professor, executive director, Banner – UMC Phoenix Advanced Lung Disease Care, and chair, clinical medicine, Banner – University Medical Group; Tony Hodges, MD, transplant pulmonologist, Banner – UMC Phoenix; and Deb Maurer, RN, statewide advanced organ and transplant management administrator at Banner – University Medicine.
Others Dr. Knoper recognized include Scott Lick, MD, UA professor of surgery and surgical director of the Heart and Lung Transplant program at Banner – UMC Tucson; Rajeev Saggar, MD, UA clinical associate professor, executive director, Banner – UMC Phoenix Advanced Lung Disease Care, and chair, clinical medicine, Banner – University Medical Group; Tony Hodges, MD, transplant pulmonologist, Banner – UMC Phoenix; and Deb Maurer, RN, statewide advanced organ and transplant management administrator at Banner – University Medicine.
Broader Geographic Reach
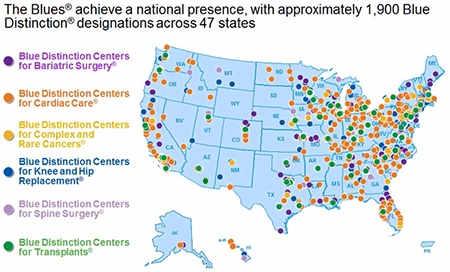
 Maurer, who heads to Houston soon for a position with Baylor St. Luke’s Medical Center, said the Blue Cross Blue Shield recognition is on a national level as opposed to Blue Cross Blue Shield of Arizona. The hospital had the state recognition previously and that was renewed when CMS re-credentialed the lung transplant program. The process for the Blue Distinction Center status began early this year, she said, and Banner Health was notified the program passed all quality standards in mid-September. Details are now in the contract negotiation phase, she added.
Maurer, who heads to Houston soon for a position with Baylor St. Luke’s Medical Center, said the Blue Cross Blue Shield recognition is on a national level as opposed to Blue Cross Blue Shield of Arizona. The hospital had the state recognition previously and that was renewed when CMS re-credentialed the lung transplant program. The process for the Blue Distinction Center status began early this year, she said, and Banner Health was notified the program passed all quality standards in mid-September. Details are now in the contract negotiation phase, she added.
 “While contracts for this are still in process, essentially, what it means is we’ll be able to expand our transplant services—which have already grown dramatically—to a broader geographical area,” Dr. Malo said. “That’s important for patients who come from other states for various reasons.”
“While contracts for this are still in process, essentially, what it means is we’ll be able to expand our transplant services—which have already grown dramatically—to a broader geographical area,” Dr. Malo said. “That’s important for patients who come from other states for various reasons.”
He noted those reasons could be either due to additional family or other support they find here or that they don’t have the caliber of program and services available in the state or area they’re from now.
“Previously that insurance might have been a barrier, but this now allows us to offer transplant services to a broader range of patients,” Dr. Malo added. “It’s just another example of the recognition of the growth and the value in the program that we’ve built.”
EXTRA INFO: Lung Transplants
What is a lung transplant?
Types of lung transplant procedures include:
- Single lung. This is the transplant of one lung.
- Double lung. This is the transplant of both lungs.
- Bilateral sequential. This is the transplant of both lungs, done one at a time. It’s also called bilateral single.
- Heart-lung transplant. This is the transplant of both lungs and the heart taken from a single donor.
- Lobar lung transplant. A rare kind of lung transplant involves this procedure from a living donor. For this surgery, a healthy adult donates a segment, or lobe, of one lung to another person. It's usually done in children.
Why might I need a lung transplant?
A lung transplant may be needed for the following conditions:
- Severe cystic fibrosis (CF). This is an inherited disease that causes problems in the glands that make sweat and mucus. It is ongoing, gets worse over time, and is usually fatal.
- Bronchopulmonary dysplasia or chronic obstructive pulmonary disease (COPD). These are lung diseases that can interfere with normal breathing.
- Pulmonary hypertension. This is increased blood pressure in the arteries of the lungs.
- Heart disease. Heart disease or heart defects that affect the lungs may need a heart-lung transplant.
- Pulmonary fibrosis. This is scarring of the lungs.
- Other diseases. Other conditions that can cause severe lung damage include sarcoidosis, histiocytosis, and lymphangioleiomyomatosis. Also, certain hereditary conditions can affect the lungs.
Not all people with these conditions need a lung transplant. A lung transplant is not advised as a treatment for lung cancer. Your healthcare provider may have other reasons to advise a lung transplant.
How many lung transplants are performed each year?
Since 1988, there have been nearly 38,000 U.S. lung transplant procedures completed and 1,250 heart/lung transplant procedures, according to the United Network for Organ Sharing (UNOS). More recently, the average is roughly 2,000 a year, significantly lower than one of the most common forms of transplant surgery for kidneys at about 18,000 a year. Lung transplants make up about 5 percent of all transplant procedures in the past three decades.How long can you live with a lung transplant?
A lung transplant can improve your quality of life and extend your lifespan. The first year after the transplant is the most critical. This is when the risk of complications is highest.In recent years, short-term survival after lung transplant has improved. Recent data from the National Heart, Lung, and Blood Institute on single-lung transplants show that:
- About 78 percent of patients survive the first year
- About 63 percent of patients survive 3 years
- About 51 percent of patients survive 5 years
Survival rates for double-lung transplants are slightly better. Recent data show that the median survival for single-lung recipients is 4.6 years. The median survival for double-lung recipients is 6.6 years. Talk with your doctor about what these figures may mean for you.
NOTE: This was originally posted on Oct. 5, 2015 at 9 a.m. It was reposted on Oct. 25, 2018 at 9:30 a.m. upon news contracts had been signed by Banner Health related to the Blue Cross Blue Shield Blue Distinction Center® designation for lung transplantation.
ALSO SEE:
“UA Lung Transplant Docs Help Banner – UMC Tucson Gain ‘Institute of Excellence’ Status with Aetna” | Posted Jan. 19, 2018
“Pulmonary Docs Thrilled with CMS Certification for Lung Transplant Program” | Posted Oct. 21, 2016
“UA Medical Center Recognized for Quality in Transplant Care” | Posted Feb. 23, 2015

