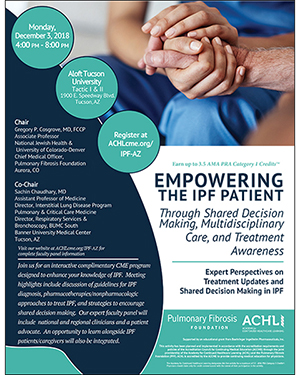
 The University of Arizona College of Medicine – Tucson—through its pulmonary division—will cohost a free event, “Empowering the IPF Patient Through Shared Decision Making, Multidisciplinary Care, and Treatment Awareness,” Dec. 3, 4-8 p.m., at Aloft Tucson University with the Pulmonary Fibrosis Foundation and the Academy for Continued Healthcare Learning.
The University of Arizona College of Medicine – Tucson—through its pulmonary division—will cohost a free event, “Empowering the IPF Patient Through Shared Decision Making, Multidisciplinary Care, and Treatment Awareness,” Dec. 3, 4-8 p.m., at Aloft Tucson University with the Pulmonary Fibrosis Foundation and the Academy for Continued Healthcare Learning.
A complimentary 3.5 AMA PRA Category 1 Credit™ value that meets policies of the Accreditation Council for Continuing Medical Education is available through a joint providership of the PFF and ACHL for attendees. This CME activity is intended for members of the care center network and surrounding regional clinicians including pulmonologists, radiologists, pathologists, respiratory nurses, respiratory therapists, and others interested in treatment advances for patients with idiopathic pulmonary fibrosis (IPF). A further patient education component will be incorporated for patients and caregivers dealing with IPF.
 The event is chaired by Gregory P. Cosgrove, MD, associate professor of medicine, assistant director of the Interstitial Lung Disease Program in the Division of Pulmonary, Critical Care and Sleep Medicine and the Endowed Chair in Interstitial Lung Disease at National Jewish Health and the University of Colorado – Denver, as well as chief medical officer of the Pulmonary Fibrosis Foundation in Aurora, Colo.
The event is chaired by Gregory P. Cosgrove, MD, associate professor of medicine, assistant director of the Interstitial Lung Disease Program in the Division of Pulmonary, Critical Care and Sleep Medicine and the Endowed Chair in Interstitial Lung Disease at National Jewish Health and the University of Colorado – Denver, as well as chief medical officer of the Pulmonary Fibrosis Foundation in Aurora, Colo.
 His co-chair is Sachin Chaudhary, MD, an assistant professor of medicine and director of the Interstitial Lung Disease Program at the UA Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, and director of Director, Respiratory Services & Bronchoscopy at Banner – University Medical Center South. The UA Pulmonary division is one of 14 in the UA Department of Medicine, one of six original and the largest department in the UA College of Medicine – Tucson.
His co-chair is Sachin Chaudhary, MD, an assistant professor of medicine and director of the Interstitial Lung Disease Program at the UA Division of Pulmonary, Allergy, Critical Care and Sleep Medicine, and director of Director, Respiratory Services & Bronchoscopy at Banner – University Medical Center South. The UA Pulmonary division is one of 14 in the UA Department of Medicine, one of six original and the largest department in the UA College of Medicine – Tucson.
If you are a patient or caregiver, call Karen Catino at (773) 714-0705 ext. 128 or visit ACHLcme.org/IPF-PT
See this link to add the event to your personal schedule (via iCal, MSOutlook, Google or Yahoo! Calendar).
Agenda
 4:00-4:05 p.m. — Welcome / Introductions | Clinician/patient/caregiver
4:00-4:05 p.m. — Welcome / Introductions | Clinician/patient/caregiver
4:05-4:15 p.m. — The Impact of IPF | Clinician
4:15-4:25 p.m. — Identifying At-risk Patients | Clinician
4:25-4:40 p.m. — Making a Differential Diagnosis | Clinician
4:40–4:55 p.m. — BREAK
4:55–5:10 p.m. — Pharmacotherapies for IPF | Clinician
 5:10–5:25 p.m. — Question and Answers | Clinician/patient/caregiver
5:10–5:25 p.m. — Question and Answers | Clinician/patient/caregiver
5:25–5:40 p.m. — Expert Updates and Insights | Clinician
5:40–6:05 p.m. — BREAK
6:05–6:25 p.m. — Multidisciplinary Approaches | Clinician/patient/caregiver
6:25–6:45 p.m. — Comprehensive Care Planning | Clinician/patient/caregiver
6:45–7:05 p.m. — Shared Decision Making | Clinician/patient/caregiver
 7:05–7:20 p.m. — Overview of IPF | Patient/Caregivers
7:05–7:20 p.m. — Overview of IPF | Patient/Caregivers
7:20–7:35 p.m. — Managing IPF | Patient/Caregivers
7:35–7:45 p.m. — Common Patient Concerns | Patient/Caregivers
7:45–8:00 p.m. — Question and Answers | Clinician/patient/caregiver
- Flyer for Clinicians:
 ipf181_pff-ahcl_az-clinician-invite_flyer_2018-v2.pdf
ipf181_pff-ahcl_az-clinician-invite_flyer_2018-v2.pdf - Flyer for Patients:
 ipf181_pff-ahcl_az-patient-invite_flyer_2018-v2.pdf
ipf181_pff-ahcl_az-patient-invite_flyer_2018-v2.pdf
Interstitial lung disease refers to a large group of disorders that cause progressive scarring of lung tissue and affects up to 200,000 people a year in the United States.
According to the American Lung Association, these disorders can be caused by long-term exposure to hazardous materials, such as asbestos, chemicals, coal dust or tobacco use. It also can be caused by an autoimmune disease, such as rheumatoid arthritis. Often the cause is unknown. Once lung scarring occurs, it's generally irreversible but effects of the damage can be slowed by certain medications. Occasionally, sufferers may be recommended for lung transplantation.
Among these disorders, idiopathic pulmonary fibrosis (IPF) is one for which a cause is largely unknown. It affects 13 to 20 people per 100,000 worldwide, with about 30,000 to 40,000 new U.S. cases diagnosed per year. Over time, the scarring gets worse and it becomes harder to take in a deep breath and the lungs cannot take in enough oxygen. Most people only survive 3-5 years after diagnosis, most commonly from respiratory failure, without a lung transplant. New therapies are being investigated—including here at the UA Health Science colleges, but currently no medicines have been shown to slow or reverse IPFs progression, according to the National Heart, Lung, and Blood Institute, a unit of the National Institutes of Health.
This event also is supported by an educational grant from Boehringer Ingelheim Pharmaceuticals, Inc.
Questions? Please contact Jacque Carrillo, (520) 621-4368 or jacqueline.carrillo@bannerhealth.com
ALSO SEE:
“Pulmonary Fibrosis Foundation Sponsors UA Lecture on Interstitial Lung Disease, Dec. 8” | Posted Nov. 30, 2017
"UA College of Medicine – Tucson’s Interstitial Lung Disease (ILD) Program Chosen to Join the National Pulmonary Fibrosis Foundation Care Center Network" | Posted Feb. 26, 2015

