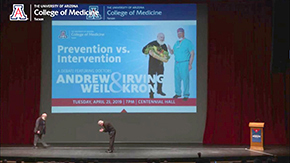
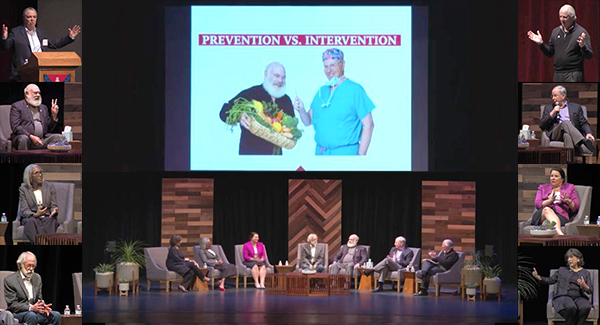
 A full house turned out for the #UAGreatDebate at the University of Arizona’s Centennial Hall on Tuesday evening, April 23, to hear cardiothoracic surgeon and interim dean of the UA College of Medicine – Tucson Irving L. Kron, MD, face off against Andrew T. Weil, MD, founder of
A full house turned out for the #UAGreatDebate at the University of Arizona’s Centennial Hall on Tuesday evening, April 23, to hear cardiothoracic surgeon and interim dean of the UA College of Medicine – Tucson Irving L. Kron, MD, face off against Andrew T. Weil, MD, founder of 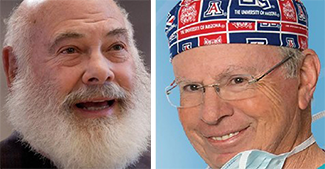 the UA Andrew Weil Center for Integrative Medicine recently renamed in his honor after a gift of $15 million to the university.
the UA Andrew Weil Center for Integrative Medicine recently renamed in his honor after a gift of $15 million to the university.
The subject: “Prevention vs. Intervention,” which better serves the patient in the modern medical era.
The event was streamed live at the college’s Facebook webpage. With an overture as the audience is seated, the real action  begins with a video about the college lasts about 12 minutes into the recording. Then, UA President Robert C. Robbins, MD, who serves as emcee, is introduced by
begins with a video about the college lasts about 12 minutes into the recording. Then, UA President Robert C. Robbins, MD, who serves as emcee, is introduced by  UA Health Sciences Senior Vice President Michael D. Dake, MD.
UA Health Sciences Senior Vice President Michael D. Dake, MD.
A cardiologist, Dr. Robbins admits that he, like most physicians, believes in prevention as well as intervention when necessary as it pertains to health care. He points out, “This is billed as a debate, but it’s kind of a pillow fight and I’m meant to be the moderator. We’ve got some interesting panelists. I’ll be sort of the referee. It’s really not a fair fight because our first speaker, Dr. Andy Weil, you all know.”
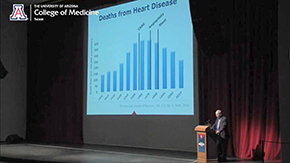
Agreeing with Dr. Robbins, Dr. Kron puts up a valiant effort aided visually by a slideshow. With two physicians on the panel (as well as Dr. Weil himself), the UA Department of Medicine is well represented. It’s an enlightening evening full of fun and informative conversation.
Much of the debate revolved around diet and exercise as key to prevention and a healthy lifestyle (an idea supported by all), but that intervention as key to when an incident or genetic predisposition cause someone’s health to go sideways, whether to get a person back on track or minimize ill effects going forward.
A big thank you to Nadia Whitehead, communications director, and Ross DuBois, special projects manager, UA College of Medicine – Tucson, and others for making the #UAGreatDebate such a wonderful event. The official attendance was 1,750.
See below for the video, a time schedule, mini-photo gallery and a few quotable highlights.
The Video
Time Schedule
To guide you through the debate, we offer the following recording guide:
- TOTAL TIME: 1:49:24
- 00:00-12:05 – Overture (feel free to skip ahead)
- 12:05-15:25 – Video about UA College of Medicine – Tucson
- 15:25-17:40 – UAHS SVP Dr. Michael Dake welcomes attendees and introduces UA President
- 17:40-20:00 – UA President Dr. Robert Robbins lays out the evening’s program
- 20:00-30-00 – Dr. Andrew Weil weighs in on ‘Prevention’
- 30:00-38:00 – Dr. Irving Kron weighs in on ‘Intervention’
- 38:00-42:00 – Rebuttals (seated)
- 42:00-43:30 – Dr. Robbins introduces panelists
- 43:30-45:30 – Comments by Roberta Diaz Brinton, PhD – director, UA Center for Innovation in Brain Science
- 45:30-49:30 – Comments by Juanita L. Merchant, MD, PhD – chief, UA Division of Gastroenterology and Hepatology, and elected member, National Academy of Medicine
- 49:30-55:00 – Comments by Nancy K. Sweitzer, MD, PhD – chief, UA Division of Cardiology; director, UA Sarver Heart Center; and editor, Circulation: Heart Failure
- 55:00-58:00 – Comments by Joaquin Ruiz, PhD – dean, UA College of Science
- 58:30-1:02:30 – Dr. Robbins explains Audience Participation portion of event, including polls and word clouds
- 1:02:30 – Audience Questions (Q&A)
- 1:49:24 – End
Mini-Photo Gallery
Click images to enlarge:
EXTRA INFO: Quotables
A few choice comments from the Q&A:
On inflammation…
“Inflammation is the cornerstone of the bodies healing response. It’s the way that the body gets more nourishment or more immune activity to an area that’s under attack. We all know it on the surface of the body. It’s redness, heat, swelling and pain. But internally, inflammation is so powerful and potentially destructive that it’s very important that it stay where it’s supposed to stay and end when it’s supposed to end. If inflammation serves no purpose, if it persists, it becomes productive of disease. You’ve got to be able to produce enough inflammation to resist infection. But, if you produce too much inflammation, you’re prone to allergies, autoimmunity and it looks as if many of the most serious chronic degenerative diseases begin as inflammatory processes. That’s true of Alzheimer’s, it’s true of coronary artery disease and there’s a link with cancer because anything that upregulates inflammation and also upregulates cell proliferation increases the risk of malignant transformation. So, you wanna contain inappropriate inflammation. There are many contributors to inflammation, genetics, stress, exposure to environmental toxins. Secondary smoke is a tremendous agent, but diet has a huge influence. And I think there’s no question that the mainstream North American diet is pro-inflammatory. It gives us the wrong kinds of fats, the wrong kinds of carbohydrates and not enough of the protective elements that are mostly found in fruits, vegetables, herbs and spices. ” — Dr. Andrew Weil
On cancer screening for the upper GI tract as opposed to colonoscopies…
“Currently, the recommendations are usually for someone diagnosed with something called Barrett’s esophagus and, actually, we know that it tends to be largely in white males. We don’t know why that is. It is considered a precancerous lesion, but in the end, probably not even 1 percent of the people who have this lesion will actually go on to develop cancer. This is the problem. We don’t know who’s going to actually develop cancer. (It’s) sort of the same issue with polyps. We don’t know which of those polyps (may become cancerous). That’s why we take them out. We don’t know which ones will actually develop into cancer. With respect to stomach cancer, we and the person who got the Nobel Prize for it know that infection for Helicobacter pylori can predispose you to gastric cancer. But only about half the people actually come with symptoms, i.e., we will see them in the clinic; and, then, only about 10 percent of those will actually develop into pre-neoplastic changes. But there are no screening guidelines for stomach cancer. There are some newer data coming out to suggest that certain minority groups, African Americans, Native Americans and possibly Hispanics, who will have a higher incidence of going on to develop cancer. So, the recommendations, although they haven’t been picked up by the insurance companies so nobody’s paying for it, (are) that perhaps we should screen those groups more often for stomach cancer.” — Dr. Juanita Merchant
On cholesterol and heart health…
“A lot of therapies aimed at decreasing bad HDLs (high-density lipoproteins) have failed. The experts in the cardiovascular field feel that the reason those fail is they just give you more of the wrong kind of HDL. So, there’s good HDLs and there’s bad HDLs and a number only tells you a small amount of the information that’s necessary to really understand the complex lipid biology. So, the short answer is that exercise and controlling weight are absolutely the best ways to give you healthy HDLs, the kind that involve good cholesterol and higher levels of it. Metabolic syndrome, higher diabetes is associated with high triglycerides and low HDL – a very bad profile. There was one study recently of a specific type of Omega 3 oil, not fish oil or the type you buy over the counter, that seemed to have a positive effect not so much to raise HDL. It was given to raise HDL, which it did, but the benefits seemed to be above and beyond that. We have a lot more to learn. Lipid biology is really complex. I’m happy to say we’ve got a clinical lipidologist starting in the cardiovascular clinic in August of this year who’s an expert on it. If you’ve got complex cholesterol, we’d be happy to set you up to see him when he gets here.” — Dr. Nancy Sweitzer
On the gut microbiome…
“There are more bacteria that live in your gut than there are cells in your body. The microbiome is a general term. We usually think of your microbiome in your GI tract. But also the microbiome are bacteria on any surface that interfaces with the environment, so your skin, genitourinary tract, the oral pharynx; it’s the microbiome in your gut, so that’s where the probiotics come in. That’s where pharmaceutical companies are trying to package up specific bacteria for you to take to try to improve your microbiome. That’s because the good bacteria will produce certain substances, particularly lactic acid and butyric acid or butyrate which keeps, specifically, your colon healthy. It’s anti-inflammatory, but we don’t know. Your body may be able to handle it better than a pill that’s packaged up that you would take.” — Dr. Juanita Merchant
“People need to know that the microbes living in your gut are a major determinant of your reactions to the environment. I think this is a key to understanding allergy, autoimmunity and a very exciting frontier is the activity of the microbiome on mental and emotional health. I think that’s just fascinating. And there’s questions about how you can alter your microbiome. I think you can do that by changing your diet, but the most practical piece of information I can give you is you should be eating fermented foods. Fermented foods are very easy to make at home. They’re cheap. I have just finished a new batch of sauer kraut, I have a new batch of pickles and kim chi, but you want to eat these things regularly and that’s probably much more effective than taking a probiotic supplement.” — Dr. Andrew Weil
ALSO SEE:
“It's Weil vs. Kron — UA doctors debate issue of medical intervention, prevention” | (Arizona Daily Star) Posted April 21, 2019
“Dr. Andrew Weil to Debate Dr. Irving Kron During Free Public Event, April 23” | (UA College of Medicine) Posted April 8, 2019
“Centennial Hall ‘Great Debate’ Spotlights Drs. Andrew Weil, Irv Kron on Prevention vs. Intervention, April 23” | Posted March 29, 2019
“Integrative Medicine Pioneer Dr. Andrew Weil Commits $15M to Name UA Center for Integrative Medicine, Bringing Total Giving to $20M” | Posted March 12, 2019