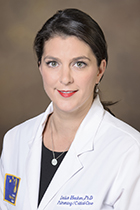
Dr. Hecker (center above) credits her success to the talented team of investigators working with her on this project. She takes pride in her “outside the box” approaches of managing her laboratory (heckerlab.arizona.edu). [Photo: Kris Hanning, UAHS Biocommunications]
 For Louise Hecker, PhD, an associate professor in the pulmonary division of the University of Arizona College of Medicine – Tucson’s Department of Medicine, research investigator with the Southern Arizona VA Health Care System and member of the UA BIO5 Institute, every breath of life is precious.
For Louise Hecker, PhD, an associate professor in the pulmonary division of the University of Arizona College of Medicine – Tucson’s Department of Medicine, research investigator with the Southern Arizona VA Health Care System and member of the UA BIO5 Institute, every breath of life is precious.
A year after coming to Tucson in 2014 from the University of Alabama at Birmingham (UAB), Dr. Hecker went back to give a eulogy at a funeral for a close friend, Gary Godwin, a 22-year U.S. Army veteran who had suffered from idiopathic pulmonary fibrosis (IPF), the subject of her research. IPF is a “disease of aging” that causes a rapid decline in respiratory function due to progressive scarring of lung tissue.
![A chest radiograph of a patient with idiopathic pulmonary fibrosis (above) along with a high resolution computed tomography scan (below) of the chest of an IPF patient that, in dark areas, shows peripheral basal pattern of coarse reticulation with honeycombing. [Credit: Wikipedia/IPFeditor] A chest radiograph of a patient with idiopathic pulmonary fibrosis (above) along with a high resolution computed tomography scan (below) of the chest of an IPF patient that, in dark areas, shows peripheral basal pattern of coarse reticulation with honeycombing. [Credit: Wikipedia/IPFeditor]](/sites/default/files/ipf-and-the-lungs-2_350x233px-96dpi.jpg) Dr. Hecker was awarded a $4.4 million U.S. Department of Defense (DoD) grant, “Preclinical Development of Small-Molecule Inhibitors Targeting Nox4 for Pulmonary Fibrosis,” to continue her work on the pre-clinical development of drug candidates for IPF.
Dr. Hecker was awarded a $4.4 million U.S. Department of Defense (DoD) grant, “Preclinical Development of Small-Molecule Inhibitors Targeting Nox4 for Pulmonary Fibrosis,” to continue her work on the pre-clinical development of drug candidates for IPF.
She also was awarded $1.5 million in additional funding last year from the National Institute of Aging, a unit of the National Institutes of Health, (NIA/NIH Award No. R21AG054766) and from the U.S. Department of Veterans Affairs (VA Merit Award No. BX003919) for other research she’s conducting related to pulmonary fibrosis.
Pictured left, a chest radiograph of a patient with idiopathic pulmonary fibrosis (above) along with a high resolution computed tomography scan (below) of the chest of an IPF patient that, in dark areas, shows peripheral basal pattern of coarse reticulation with honeycombing. [Credit: Wikipedia/IPFeditor]
The DoD award is part of a larger effort in recent years by the military through its Congressionally Directed Medical Research Programs to address respiratory illnesses that disproportionately affect veterans, including pulmonary fibrosis, tuberous sclerosis and lung cancer.
EXTRA INFO
Dr. Louise Hecker was a guest Sept. 6, 2018, on KUAZ 89.1 FM during the AZPM News portion of NPR’s Morning Edition radio broadcast.
You can read about — and listen to her interview with Arizona Public Media producer Tony Paniagua — here: “Grant Funds Research to Fight Deadly Lung Disease.”
According to the Pulmonary Fibrosis Foundation, IPF affects one of every 200 U.S. adults—largely men—over age 65, with 40,000 people dying from it each year. The foundation has named the UA College of Medicine – Tucson and Banner – University Medical Center Tucson to its National PFF Care Center Network.
![From left: YoonJoo Shin, Dr. Louise Hecker, and Dr. Sabbir Khan. [Credit: Kris Hanning, UAHS Biocommunications] From left: YoonJoo Shin, Dr. Louise Hecker, and Dr. Sabbir Khan. [Credit: Kris Hanning, UAHS Biocommunications]](/sites/default/files/hecker-lab_yoon-sabbir-and-dr.-hecker_450x300px-96dpi.jpg) At right, Dr. Hecker discussing research data with members of her lab, YoonJoo Shin and Sabbir Khan, PhD.
At right, Dr. Hecker discussing research data with members of her lab, YoonJoo Shin and Sabbir Khan, PhD.
“A factoid that always shocks people is that about 45 percent of deaths in the U.S. each year are attributed to scar-tissue-related diseases,” Dr. Hecker said. “But the reason most people are not aware of this alarming statistic is because the ‘cause of death’ is organ failure, and organ failure is often the result of progressive scar tissue. End-stage heart failure, for instance, typically results from progressive scar tissue in the heart. I study the most relentless and fatal disease of tissue scarring which happens in the lungs.”
“Currently, there are two drugs approved by the U.S. Food and Drug Administration for IPF,” she added, “but they are not a ’cure‘ and they do not improve the quality of life for IPF patients.”
Regenerative Roots
A New York native, Dr. Hecker earned a bachelor’s degree in biology from Hartwick College and a master’s degree in ecology, evolution and behavior from Binghamton University, where among things she studied were tissue regenerative properties of amphibians. She went on to complete another master’s degree in cell and developmental biology and a doctorate in applied physics at the University of Michigan, where her work focused on developing bioartificial tissues.
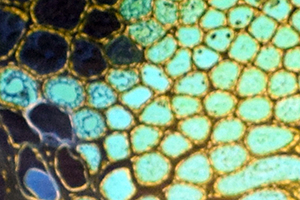 A framed image of turquoise scales (left) hangs on Dr. Louise Hecker’s UA office wall—a magnified view of a salamander’s tail glands. During her earliest research experiences, she studied regenerative properties of amphibians that informs her work on lung reparative properties. Amphibians regrow damaged parts, while humans’ reaction to injury is to form scars. “Having training in development and regeneration helps me to better understand aging and the lack of repair that occurs as we get older,” she said.
A framed image of turquoise scales (left) hangs on Dr. Louise Hecker’s UA office wall—a magnified view of a salamander’s tail glands. During her earliest research experiences, she studied regenerative properties of amphibians that informs her work on lung reparative properties. Amphibians regrow damaged parts, while humans’ reaction to injury is to form scars. “Having training in development and regeneration helps me to better understand aging and the lack of repair that occurs as we get older,” she said.
 At Michigan, she also completed a post-doctoral fellowship in lung injury-repair responses, where she was the lead author on the research team that was the first to identify a critical role for the oxidant-generating enzyme, Nox4, as a key mediator in regulating scar tissue in the lung. The study further demonstrated that Nox4 overexpression is significantly elevated in IPF patient lungs, which may be the cause of excessive lung scarring in these patients (see "NADPH oxidase-4 mediates myofibroblast activation and fibrogenic responses to lung injury," Nature Medicine, September 2009).
At Michigan, she also completed a post-doctoral fellowship in lung injury-repair responses, where she was the lead author on the research team that was the first to identify a critical role for the oxidant-generating enzyme, Nox4, as a key mediator in regulating scar tissue in the lung. The study further demonstrated that Nox4 overexpression is significantly elevated in IPF patient lungs, which may be the cause of excessive lung scarring in these patients (see "NADPH oxidase-4 mediates myofibroblast activation and fibrogenic responses to lung injury," Nature Medicine, September 2009).
Nox enzymes, Dr. Hecker noted, are crucial to our bodies’ natural ability to protect and heal themselves, including mechanisms of inflammation and scar tissue. Without the capability to develop scar tissue, we wouldn’t be able to repair tissue injury. Since Dr. Hecker’s original finding that Nox4 mediates scar tissue in the lungs, hundreds of studies that followed have demonstrated that it is a key regulator of scar tissue in many other organs, including the heart, skin, kidney and liver.
 From Michigan, Dr. Hecker joined UAB’s faculty in 2009, where she became interested in understanding why normal repair processes “go awry” in aging. The problem as we age is that our bodies’ ability to efficiently repair itself declines, she said. Progressive scar tissue that can become fatal is a hallmark of aging in many organ systems. Dr. Hecker’s work showed that, in aging, Nox4 becomes dysfunctional—as if the switch to “turn off” Nox4 is broken, so it remains “turned on” leading to excessive scar tissue formation (see “Reversal of Persistent Fibrosis in Aging by Targeting NOX4-Nrf2 Redox Imbalance,” Science Translational Medicine, April 2014). While at UAB, she also won a small grant to develop a screening assay for Nox4 to allow faster evaluation of 30,000 potential drug candidates for treating IPF.
From Michigan, Dr. Hecker joined UAB’s faculty in 2009, where she became interested in understanding why normal repair processes “go awry” in aging. The problem as we age is that our bodies’ ability to efficiently repair itself declines, she said. Progressive scar tissue that can become fatal is a hallmark of aging in many organ systems. Dr. Hecker’s work showed that, in aging, Nox4 becomes dysfunctional—as if the switch to “turn off” Nox4 is broken, so it remains “turned on” leading to excessive scar tissue formation (see “Reversal of Persistent Fibrosis in Aging by Targeting NOX4-Nrf2 Redox Imbalance,” Science Translational Medicine, April 2014). While at UAB, she also won a small grant to develop a screening assay for Nox4 to allow faster evaluation of 30,000 potential drug candidates for treating IPF.
The Lure of Expertise (and a Friend)
In 2014, Dr. Hecker was recruited to the UA under the leadership of then-UA Health Sciences senior vice president Joe G.N. “Skip” Garcia, MD, a leading authority on the genetic basis of lung disease and the prevention and treatment of inflammatory lung injury. Dr. Garcia is a member of her DoD study’s advisory board, which also includes the UA College of Pharmacy’s Laurence Hurley, PhD; UA Professor of Medicine and Associate Dean of Faculty Affairs and Development at the UA College of Medicine – Phoenix Ken Knox, MD; the UA Center for Accelerated BioMedical Innovation’s Marvin Slepian, MD, and Rakhi Gibbons, of Tech Launch Arizona—the commercialization arm of the university which helps bring UA-developed innovations to market.
 Another member is the patient advocate Susan Godwin, the widow of Gary Godwin, who was diagnosed with IPF. Dr. Hecker met the Godwins (pictured right) when Gary was in a clinical trial for advanced lung disease at UAB Hospital. In 2010, after several false starts, he got a lung transplant there.
Another member is the patient advocate Susan Godwin, the widow of Gary Godwin, who was diagnosed with IPF. Dr. Hecker met the Godwins (pictured right) when Gary was in a clinical trial for advanced lung disease at UAB Hospital. In 2010, after several false starts, he got a lung transplant there.
 “In a very short time, this 60-something couple had become my extremely close friends,” Dr. Hecker acknowledges. “I was devastated when he died. Yes, it’s sad—but, on the other hand, Gary did beat the odds. Less than 50 percent of lung transplant patients survive five years, and Gary made it beyond that point.”
“In a very short time, this 60-something couple had become my extremely close friends,” Dr. Hecker acknowledges. “I was devastated when he died. Yes, it’s sad—but, on the other hand, Gary did beat the odds. Less than 50 percent of lung transplant patients survive five years, and Gary made it beyond that point.”
Susan, founder of Christian Copyright Solutions in Fairhope, Ala., said she is happy to be able to contribute. “I'm thrilled to serve as a patient advocate for this exciting project,” she said.
“Susan’s role on the advisory board is to speak to the challenges an IPF patient might face with an inhaled therapy, given this is a disease where patients already have trouble breathing,” Dr. Hecker said.
Part of what attracted Dr. Hecker to the UA was the medicinal chemistry and drug development expertise here. With further financial support from the BIO5 Institute, she was able to assemble a team to continue pre-clinical development and testing of novel drug candidates identified at the UA. Patents were filed for two different classes of promising IPF drug candidates.
Narrowing in on a Solution
![MinJin Kang, PhD, and chemistry student Joseph Irish conduct research in the lab of Louise Hecker. [Credit: Kris Hanning, UAHS Biocommunications] MinJin Kang, PhD, and chemistry student Joseph Irish conduct research in the lab of Louise Hecker. [Credit: Kris Hanning, UAHS Biocommunications]](/sites/default/files/hecker-lab_minjin-and-joey_375x250px-96dpi.jpg) Now, with the DoD grant, Dr. Hecker and her team will push four aims to develop an effective therapy to halt IPF’s progression and more importantly, to reverse it. The first is to optimize medicinal chemistry on drug candidates; next is to develop and evaluate novel formulations for both oral and inhaled methods of administration; third, they will evaluate those candidates for safety and efficacy in animal models; and, finally, the lead drug candidate will be tested in larger animal models. That fourth aim is an FDA requirement prior to consideration for human clinical trials. Those tests will be performed atLovelace Respiratory Research Institute (Albuquerque, NM) Lovelace, Dr. Hecker points out, is the largest respiratory pre-clinical contract research organization in the country.
Now, with the DoD grant, Dr. Hecker and her team will push four aims to develop an effective therapy to halt IPF’s progression and more importantly, to reverse it. The first is to optimize medicinal chemistry on drug candidates; next is to develop and evaluate novel formulations for both oral and inhaled methods of administration; third, they will evaluate those candidates for safety and efficacy in animal models; and, finally, the lead drug candidate will be tested in larger animal models. That fourth aim is an FDA requirement prior to consideration for human clinical trials. Those tests will be performed atLovelace Respiratory Research Institute (Albuquerque, NM) Lovelace, Dr. Hecker points out, is the largest respiratory pre-clinical contract research organization in the country.
 Serving as co-investigators on the DoD study are Phil Kuehl, PhD, Lovelace’s director of scientific core laboratories, and the UA’s Vijay Gokhale, PhD, Heidi Mansour, PhD, and Brett Colson, PhD.
Serving as co-investigators on the DoD study are Phil Kuehl, PhD, Lovelace’s director of scientific core laboratories, and the UA’s Vijay Gokhale, PhD, Heidi Mansour, PhD, and Brett Colson, PhD.
Dr. Colson is a UA College of Medicine – Tucson assistant professor of cellular and molecular medicine, Dr. Mansour is a UA College of Pharmacy assistant professor and Dr. Gokhale is the director of computational chemistry at the BIO5 Institute’s Drug Discovery and Development Center. BIO5 funding allowed Dr. Hecker to recruit a medicinal chemist, Reena Chawla, PhD, who was instrumental in working on the chemistry team with Dr. Gokhale and identifying the lead drug candidates. Gajanan Inamdar, PhD, subsequently joined the medicinal chemistry team, headed by Dr. Gokhale. Dr. Colson, a biophysicist, will work closely with the chemistry team to ensure that the drug candidates bind tightly with Nox4 to achieve maximal potency. “It is exciting to learn how the drug candidates alter Nox4 function at the molecular level,” said Dr. Colson. “This is key to understanding how these drug candidates work.” The team will also develop optimized formulations for oral and inhaled drug administration. This may be unique to each compound, since Dr. Hecker’s identified leads suggest that one may work better as an oral drug whereas the other class of drug candidates seem better suited for inhaled delivery.
“We’re going to test if it works and if it’s safe,” Dr. Hecker said, referring to efficacy and toxicology screening. “Before you give these drug candidates to human patients in clinical trials, we have to perform rigorous, controlled testing to evaluate both. Dr. Kuehl, who heads the team at Lovelace, will play an important role to evaluate the safety of our top candidates, an FDA requirement that is necessary in order to initiate clinical trials later.”
Dr. Gokhale said, “I am confident that our team will be able to meet the goal of developing a therapy for effective treatment of this disease.”
Above and Beyond
![Dr. Louise Hecker's lab team outside the University of Arizona BIO5 Institute [Credit: Kris Hanning, UAHS Biocommunications] Dr. Louise Hecker's lab team outside the University of Arizona BIO5 Institute [Credit: Kris Hanning, UAHS Biocommunications]](/sites/default/files/hecker-lab_team-shot_375x250px-96dpi.jpg) The successful development of a first-in-class selective Nox4 inhibitor could have profound healthcare impacts, Dr. Hecker underscored.
The successful development of a first-in-class selective Nox4 inhibitor could have profound healthcare impacts, Dr. Hecker underscored.
 In her most recent studies, Dr. Hecker’s team has demonstrated Nox4 may play a role in other age-related lung diseases, including acute respiratory distress syndrome (ARDS) that involves widespread lung inflammation in critically ill patients. These findings appeared in the American Journal of Physiology - Lung Cellular and Molecular Physiology’s March 2017 issue (see "Dysregulated Nox4 ubiquitination contributes to redox imbalance and age-related severity of acute lung injury"). “This is exciting because it suggests the drug candidates that we are developing for IPF may also provide therapeutic benefit to other patient populations,” Dr. Hecker said. There are currently no FDA-approved drug treatments for ARDS. Nox4 targeting drugs could provide a first-in-class treatment option for ARDS patients.
In her most recent studies, Dr. Hecker’s team has demonstrated Nox4 may play a role in other age-related lung diseases, including acute respiratory distress syndrome (ARDS) that involves widespread lung inflammation in critically ill patients. These findings appeared in the American Journal of Physiology - Lung Cellular and Molecular Physiology’s March 2017 issue (see "Dysregulated Nox4 ubiquitination contributes to redox imbalance and age-related severity of acute lung injury"). “This is exciting because it suggests the drug candidates that we are developing for IPF may also provide therapeutic benefit to other patient populations,” Dr. Hecker said. There are currently no FDA-approved drug treatments for ARDS. Nox4 targeting drugs could provide a first-in-class treatment option for ARDS patients.
“Heart failure is another major killer in the United States. We can manage the complications following a heart attack, but we have no drug that addresses the progressive scar tissue of your heart that ensues, a key component of end-stage heart failure,” she added. “Our Nox4 inhibitors could potentially address this unmet health burden.”
With her work, Dr. Hecker hopes to relieve others of the burden of struggle that her friends, the Godwins suffered through prior to Gary Godwin’s death in 2015.
This work was supported by the Office of the Assistant Secretary of Defense for Health Affairs, through the Peer Reviewed Medical Research Program under Award No. W81XWH-17-1-0443. Opinions, interpretations, conclusions and recommendations are those of the author and are not necessarily endorsed by the U.S. Department of Defense.
ALSO SEE:
"UA Researchers to Study, Test Potential Drug Candidates for Deadly Lung Disease" | Posted Sept. 5, 2018
“UA Researchers Develop Novel ‘Lung-on-a-Leaf’ Model to Study Pulmonary Diseases” | Posted June 20, 2018
“Drs. Vanderpool, Knox Among 14 to Win ABRC Grant Awards Worth Total of Over $5.92 Million” | Posted April 24, 2018
“I-Squared Awards Honor Inventors, Entrepreneurs at 5th Tech Launch Arizona Event” | Posted April 3, 2018
“UA Researchers to Evaluate New Therapeutic Platform in Targeted Treatment of Idiopathic Pulmonary Fibrosis” | Posted May 31, 2017
"DOM Research Seminar to Spotlight Sleep Medicine, Novel Therapeutics for Fibrotic Diseases" | Posted Oct. 26, 2016
"Pulmonary Researcher Dr. Louise Hecker Joins UA College of Medicine – Tucson" | Posted April 14, 2014



