Just named a national Health and Aging Policy Fellow, Lisa O’Neill, DBH, MPH, has focused on many issues on behalf of older adults—hoarding disorder, elder abuse, caregiver support and effective training of a geriatrics workforce in Arizona. She’s done this as a staffer at the University of Arizona Center on Aging (since 2009), a volunteer advocate with area and state agencies, and faculty member in the UA Geriatrics division at the UA College of Medicine – Tucson (since 2018).
An Advocate for Older Adults
 To illustrate her level of involvement, Dr. O’Neill recently submitted the Sunset Review Report to the Arizona State Legislature for the 10-year renewal of the statute that supports the Governor’s Advisory Council on Aging, which works closely with the Governor’s Office on Aging. The purpose of the council is to advise the governor, legislature and state departments on all matters and issues relating to aging, including administration of the State Plan on Aging. As council chair, she normally would co-author the report with the Office on Aging’s executive director, but that position has been vacant since January.
To illustrate her level of involvement, Dr. O’Neill recently submitted the Sunset Review Report to the Arizona State Legislature for the 10-year renewal of the statute that supports the Governor’s Advisory Council on Aging, which works closely with the Governor’s Office on Aging. The purpose of the council is to advise the governor, legislature and state departments on all matters and issues relating to aging, including administration of the State Plan on Aging. As council chair, she normally would co-author the report with the Office on Aging’s executive director, but that position has been vacant since January.
She looks forward to hearings this fall which will determine if the council sunsets or is successfully renewed.
“Arizona has a long history of valuing our older adult population. Renewing the council will send a strong message that we honor this population, appreciate everything they bring to the state, and we will work together to address their unique needs and concerns. Older adults deserve to be represented in a nonpartisan manner.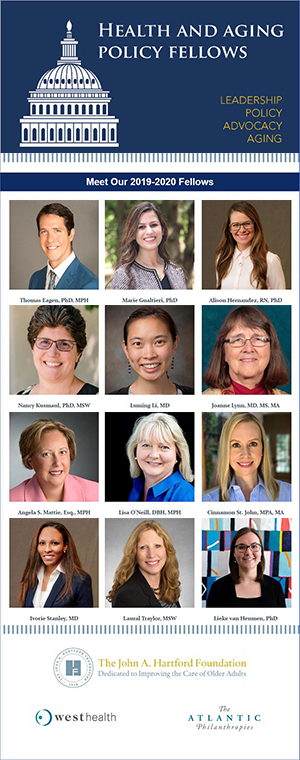 Our state needs an Office on Aging and a Governor’s Advisory Council on Aging. They are two different entities, and both are needed to support Arizona’s diverse, often vulnerable older adult population,” Dr. O’Neill said.
Our state needs an Office on Aging and a Governor’s Advisory Council on Aging. They are two different entities, and both are needed to support Arizona’s diverse, often vulnerable older adult population,” Dr. O’Neill said.
Click on the image at left to learn more about all of this year's class of Health and Aging Policy Fellows.
Class of 2020 H&A Policy Fellows
Now joining as one of a dozen 2019-20 Health and Aging Policy Fellows chosen by the National Program Office, based at Columbia University, she also looks forward to traveling to the nation’s capital—later in September—for her orientation to that program.
Established in 2008 with funding from the John A. Hartford Foundation, Atlantic Philanthropies and West Health, the Health and Aging Policy Fellows Program trains future leaders to influence health-care policy, systems and program development in aging. After a rigorous training in Washington, DC, fellows are placed for up to a year in the executive, legislative or judicial branch of government, at a federal agency, state or community agency or committee, or with a nongovernmental organization.
 “We are thrilled that Dr. Lisa O’Neill was selected for this prestigious fellowship from a national group of outstanding scholars and practitioners,” said Mindy Fain, MD, a professor of medicine, Geriatrics division chief, UA Center on Aging co-director and the Anne and Alden Hart Endowed Chair in Medicine at the UA College of Medicine – Tucson. “This fellowship is designed to develop leaders who are committed to changing policy to improve the lives of older Americans, and we are confident that Dr. O’Neill will make a significant impact locally and nationally.”
“We are thrilled that Dr. Lisa O’Neill was selected for this prestigious fellowship from a national group of outstanding scholars and practitioners,” said Mindy Fain, MD, a professor of medicine, Geriatrics division chief, UA Center on Aging co-director and the Anne and Alden Hart Endowed Chair in Medicine at the UA College of Medicine – Tucson. “This fellowship is designed to develop leaders who are committed to changing policy to improve the lives of older Americans, and we are confident that Dr. O’Neill will make a significant impact locally and nationally.”
In late October, Dr. O’Neill returns to DC for a longer six-week, in-depth orientation involving the federal legislative process as well as relevant agencies that oversee related aging and health policy. Afterward, she will be paired with an agency for a policy project to complete during the year-long fellowship.
“I’m really interested in a couple of things. As the chair of the Governor’s Council Advisory Council on Aging, I am excited to expand my skills related to advocating for older adults and creating effective and efficient policy to help improve their lives,” she said.
Behavioral Health & Primary Care
Dr. O’Neill also is interested in policy-related caregiver issues and integration of behavioral health into primary care for treatment of older adults.
“You really need to treat the whole person. If you just treat the physical conditions and ignore the mental health conditions, you’re not really fixing the whole person.”
As an example, Dr. O’Neill noted, if a person has diabetes or heart failure and the treatment plan doesn’t address the related depression or anxiety that often accompany these diseases, the patient’s overall health outcomes might suffer. Behavioral health needs to be part of the treatment plan—for both patients and caregivers. Having behavioral health providers onsite, in the primary care setting, provides the opportunity for a “warm handoff.”
“When the physician can walk the patient or caregiver down the hall to personally introduce them to a behavioral health provider, and ask ‘Why don’t you talk for a few minutes,’ the odds dramatically increase that the patient or caregiver will continue seeing the behavioral health provider. Without that ‘warm handoff,’ the odds of them seeking out yet another appointment is remote. This is especially true with older adults, who often already have financial and transportation concerns related to their medical care. They also might resist getting mental health support because they didn’t grow up with it being commonplace and may view it as unnecessary,” said Dr. O’Neill.
Dr. O’Neill is an assistant professor of medicine in the Division of Geriatrics, General Internal Medicine and Palliative Medicine at the UA College of Medicine – Tucson, the research and education associate director at the UA Center on Aging, manager of the center’s Arizona Geriatrics Workforce Enhancement Program funded by the Health Resources and Services Administration, and a 2016 UA Aging & Cognition Scholar with the center and the Healthy Brain Research Network at the U.S. Centers for Disease Control and Prevention.
EXTRA INFO: “Aging in America – A Caregiver’s Dilemma”
By 2030, 71 million Americans—about 20 percent of the U.S. population—will be age 65 and older. These individuals are at high risk for complex health problems, chronic illness, and disability, and they are, and will continue to be, the heaviest users of health care.
And as, today, older adults already make up a substantial portion of hospital days, ambulatory adult primary care visits, home care visits, and nursing home residents, we can anticipate that will only rise with projected older American population projections.
Meanwhile, more than 40 million caregivers provide 40 billion hours of unpaid care a year—an estimated $375 billion economic value. They spend an average of $7,000 a year in out-of-pocket expenses, often nearly 20 percent of their annual income. A third of them are over age 65 and go without routine physical or dental visits themselves, while suffering from at least one chronic condition.
The Health and Aging Policy Fellows Program, with 128 current and alumni fellows and 12 incoming fellows for 2019-20, focuses on enlisting outstanding scholars and practitioners from across a range of disciplines to shape policies for older Americans that address those challenges.
Learn more from the following articles:
- “Leadership for Addressing Aging in America: The Health and Aging Policy Fellowship” | Journal of the American Medical Directors Association (JAMDA), 18 (2017), pp. 819-825
- “Health and Aging Policy Fellows Program: Shaping a Healthy Future for Older Americans” | Journal of the American Geriatrics Society, September 2017, 65(9):2088-2093.
ALSO SEE:
“UA Center on Aging Staff Op-Ed Takes Aim at Elder Abuse, Social Isolation of Older Adults” | Posted June 10, 2019
“Family Caregiver Day at the Capitol, March 21, Offers Opportunity to Advocate for Elderly” | Posted March 28, 2019
“Advances in Aging Spring Lectures Kickoff Jan. 14 with Dr. Lisa O’Neill on ‘Hoarding Disorder’” | Posted Dec. 20, 2018
“UA Center on Aging Awarded Grant to Continue End-of-Life Education with Medical Students” | Posted Aug. 21, 2017
“Center on Aging Three in the News on Elder Abuse, Biological Sciences and Hearing Loss” | Posted Dec. 7, 2016
“Lisa O’Neill Named ‘2015 Gerontologist of the Year’ by Arizona Geriatrics Society” | Posted Nov. 2, 2015


