 University of Arizona Department of Medicine physicians can count another kudo for the care they provide at Banner – University Medical Center Tucson and South with the recent naming of university research and hospital clinical facilities as a “Scleroderma Research and Treatment Center” by the Scleroderma Foundation.
University of Arizona Department of Medicine physicians can count another kudo for the care they provide at Banner – University Medical Center Tucson and South with the recent naming of university research and hospital clinical facilities as a “Scleroderma Research and Treatment Center” by the Scleroderma Foundation.
The achievement is a joint effort involving multiple divisions, but primarily the Divisions of Pulmonary, Allergy, Critical Care and Sleep Medicine (PACCS), and Rheumatology. It is only the second such center in the state, the other being at the Mayo Clinic in Scottsdale. In the Southwest, other Scleroderma Foundation recognized centers exist at the University of Colorado, University of Utah and UCLA.
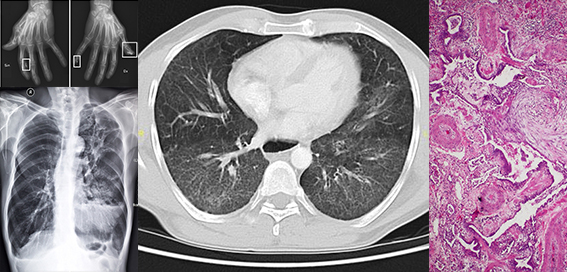
Image above right, collage of different physical impacts from systemic sclerosis (SSc), or scleroderma: On left below, pulmonary fibrosis—or scarring of the lungs—resulting from scleroderma. Left above, calcinosis of the hands as a result of CREST syndrome, also known as the limited cutaneous form of SSc. Center, “interstitial pneumonia with autoimmune features” (IPAF). Right, the most frequent pulmonary lesions in scleroderma are pulmonary hypertensive arteriopathy and interstitial pneumonia most often resembling UIP (usual interstitial pneumonia). Either or both these lesions can be present—in the case of this image, both are. (Images courtesy of Pulmonary Fibrosis News/Mikael Häggström, MD/Radiopaedia/Yale Rosen Collection on Flickr)
Another Feather
 “This is another feather in the cap for our Interstitial Lung Disease Program, which is rapidly making progress in advanced care for patients with this difficult to treat condition,” said Sairam Parthasarathy, MD, UA professor of medicine and interim chief of the pulmonary division. “It is a multidisciplinary effort with rheumatologists here, and we are delighted that it received the recognition of the Scleroderma Foundation as a stamp of excellence in the care that we provide to patients with scleroderma related lung diseases.”
“This is another feather in the cap for our Interstitial Lung Disease Program, which is rapidly making progress in advanced care for patients with this difficult to treat condition,” said Sairam Parthasarathy, MD, UA professor of medicine and interim chief of the pulmonary division. “It is a multidisciplinary effort with rheumatologists here, and we are delighted that it received the recognition of the Scleroderma Foundation as a stamp of excellence in the care that we provide to patients with scleroderma related lung diseases.”
For all research and treatment centers recognized by the Scleroderma Foundation by state, click here.
The UA/Banner program will be added next week, said Sachin Chaudhary, MD, a UA assistant professor of medicine, director of the Interstitial Lung Disease (ILD) Program and co-director of Scleroderma Research and Treatment Center. ILDs can be the manifestation of a group of disorders, including scleroderma, sarcoidosis and idiopathic pulmonary fibrosis, that cause progressive scarring of lung tissue. The ILD Program also was recognized last fall as a center of excellence by the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG).
More Referrals & Trials
 “This means more referrals for us. It will give patients in Southern Arizona a place where they can actually go and feel more confident about reliability of the care they receive. In addition, the designation means we’ll be able to conduct more clinical trials and more research in these areas,” Dr. Chaudhary added.
“This means more referrals for us. It will give patients in Southern Arizona a place where they can actually go and feel more confident about reliability of the care they receive. In addition, the designation means we’ll be able to conduct more clinical trials and more research in these areas,” Dr. Chaudhary added.
 That research and clinical care capability was boosted last fall with the arrival of the other co-director of the Scleroderma Research and Treatment Center, Alicia Rodriguez-Pla, MD, PhD, MPH, who spoke Feb. 16 at the Living Healthy With Arthritis Annual Conference, hosted in Tucson by the UA Arthritis Center, on “The Latest Advancements in the Treatment of Scleroderma.” She trained at the Universidad de Navarra in Pamplona, Spain, where she earned her medical degree, and the Universitat Autònoma de Barcelona, where she earned her doctorate. She also has received advanced training in vasculitis and scleroderma at Johns Hopkins University in Baltimore, the Baylor Institute for Immunology Research in Dallas, and the Boston Medical Center, affiliated with Boston University.
That research and clinical care capability was boosted last fall with the arrival of the other co-director of the Scleroderma Research and Treatment Center, Alicia Rodriguez-Pla, MD, PhD, MPH, who spoke Feb. 16 at the Living Healthy With Arthritis Annual Conference, hosted in Tucson by the UA Arthritis Center, on “The Latest Advancements in the Treatment of Scleroderma.” She trained at the Universidad de Navarra in Pamplona, Spain, where she earned her medical degree, and the Universitat Autònoma de Barcelona, where she earned her doctorate. She also has received advanced training in vasculitis and scleroderma at Johns Hopkins University in Baltimore, the Baylor Institute for Immunology Research in Dallas, and the Boston Medical Center, affiliated with Boston University.
“The designation of a Scleroderma Research and Treatment Center at Banner – University Medical Center by the Scleroderma Foundation is a great achievement and demonstrates national recognition of the excellent multi-disciplinary collaborations in research and clinical care that we provide to scleroderma patients,” said C. Kent Kwoh, MD, UA Arthritis Center director, chief of the Division of Rheumatology, the Charles A.L. and Suzanne M. Stephens Endowed Chair in Rheumatology and a professor of medicine and medical imaging.
 “These patients often have complex multi-system disease that requires a coordinated team approach with input from rheumatologists, pulmonologists, gastroenterologists, nephrologists, cardiologists, dermatologists, vascular surgeons and neurosurgeons,” Dr. Kwoh added.
“These patients often have complex multi-system disease that requires a coordinated team approach with input from rheumatologists, pulmonologists, gastroenterologists, nephrologists, cardiologists, dermatologists, vascular surgeons and neurosurgeons,” Dr. Kwoh added.
Dr. Rodriguez-Pla underscored Dr. Kwoh’s point by adding patients into his equation. "ln my opinion, scleroderma is one of the autoimmune diseases that is in need of further investigation to develop new therapies. Collaboration between patients and physicians is crucial for developing successful anti-fibrotic therapies. We are hopeful that by being recognized as a center for the treatment of scleroderma, more patients will come to us to establish a fruitful relationship and mutual collaboration," she said.
The Scleroderma Research and Treatment Center is part of the UA Arthritis Center, the only “center of excellence” in the state of Arizona dedicated specifically to arthritis, rheumatic and musculoskeletal disorders, and the UA Division of Pulmonary, Allergy, Critical Care and Sleep Medicine.
What Is Scleroderma?
Scleroderma, or systemic sclerosis (SSc), is a chronic connective tissue disease generally classified as one of the autoimmune rheumatic diseases. Symptoms include tightening of the skin, joint pain, exaggerated response to cold (i.e., Raynaud's syndrome) and heartburn, according to the foundation.
It involve the skin, esophagus, gastrointestinal tract (stomach and bowels), lungs, kidneys, heart and other internal organs, as well as blood vessels, muscles and joints. The tissues of involved organs become hard and fibrous, causing them to function less efficiently.
Estimates vary from 50,000 to 300,000 people suffering from scleroderma in the United States, mostly women between the ages of 30 and 50. The American College of Rheumatology pegs the figure at between 75,000 and 100,000. The condition is incurable but can be treated to mitigate symptoms particularly with early diagnoses. It’s important to recognize and treat organ involvement early on to prevent irreversible damage.
Up to 90 percent of people with scleroderma may develop some level of scarring in the lungs, due to pulmonary hypertension that frequently accompanies the disease. Known as pulmonary fibrosis, this scarring can limit daily activities because it reduces lung capacity, making it harder to breathe. It also is one of the leading causes of death in people with scleroderma.
EXTRA INFO: Scleroderma or Systemic Sclerosis
Scleroderma News: “How Scleroderma and Pulmonary Hypertension Are Related”
- Medpage Today: “Quality of Life Poor in Scleroderma”
- WebMD: “Scleroderma: Main Types & Top Questions Answered”
- HealthLine: “Systemic Sclerosis (Scleroderma)”
- MedlinePlus: “Scleroderma”
- NIH/National Institute of Arthritis and Musculoskeletal and Skin Diseases: “Scleroderma”
- NIH/U.S. National Library of Medicine/Genetics Home Reference: “Systemic scleroderma”
ALSO SEE:
“‘The Power of Precision Medicine’ Theme of Living Healthy With Arthritis Conference, Feb. 16” | Posted Jan. 17, 2019
“Banner – UMC Tucson Included in Expansion of Early Access Program for Idiopathic Pulmonary Fibrosis Genomic Classifier” | Posted Dec. 7, 2018
“Global Respiratory Alliance Names UA Interstitial Lung Disease Program among Designated 'WASOG Sarcoidosis Clinics’” | Posted Nov. 30, 2018
“Scleroderma and Vasculitis Specialist Dr. Alicia Rodriguez-Pla Joins UA Rheumatology Faculty” | Posted Sept. 20, 2018

